Breaking News


Popular News


Explore the ethical implications of using augmented reality in medicine, including patient privacy, informed consent, doctor-patient relationship, and equitable access considerations.Augmented reality (AR) has made significant strides in the field of medicine, with the potential to revolutionize the way healthcare is delivered. By superimposing digital information onto the real world, AR technology has the ability to enhance medical training, improve surgical precision, and facilitate more accurate diagnoses. However, with these advancements come a host of ethical considerations that need to be carefully examined.
In this blog post, we will delve into the ethical implications of using augmented reality in medicine, focusing on several key areas of concern. We will explore the potential impact of AR on patient privacy, the implications for obtaining informed consent, and its effect on the doctor-patient relationship. Additionally, we will consider the ethical considerations for ensuring equitable access to AR technology in healthcare. By addressing these complex ethical issues, we can better understand the responsible use of augmented reality in medicine and work towards harnessing its potential for the greater good.
Contents

Augmented reality (AR) is a groundbreaking technology that is beginning to revolutionize the field of medicine. It involves the integration of digital information and virtual objects into the real world, enhancing the perception of the physical environment. In the medical field, AR has the potential to transform the way healthcare professionals diagnose, treat, and interact with patients.
With AR, medical practitioners can access real-time information and visualize data directly within their field of vision. This invaluable tool can assist in surgical navigation, medical training, and patient education. By overlaying digital images onto the physical world, doctors can gain a better understanding of complex anatomy and pathology, leading to more accurate diagnoses and personalized treatment plans.
In addition, AR technology has the ability to improve patient outcomes and reduce medical errors. For example, surgeons can use AR to precisely map out incision points and critical structures during complex procedures, ultimately enhancing safety and efficiency in the operating room. Furthermore, patients can benefit from AR-enhanced rehabilitation and therapy programs, which can help improve their recovery process and overall well-being.
As the use of AR in medicine continues to grow, it is crucial for healthcare professionals to familiarize themselves with this innovative technology and understand its potential ethical implications. While the benefits of AR in healthcare are numerous, it is essential to carefully consider the ethical considerations and potential risks associated with its use, particularly in regards to patient privacy, informed consent, and the doctor-patient relationship.
When it comes to using augmented reality (AR) in the field of medicine, there are various ethical concerns that come into play. One of the most pressing issues is the patient privacy and the potential risks that AR technology may pose to it.
With AR, medical professionals are able to access and display patient information in real time, which can be beneficial for accurate diagnosis and treatment. However, this also raises concerns about the security of the data being shared and stored within the AR systems.
Furthermore, there is the risk of unauthorized access to patient data, as well as the potential for data breaches and leaks. This brings into question the ethical responsibility of healthcare providers and developers to ensure the privacy and confidentiality of patient information when using AR technology.
It is essential for healthcare organizations to establish strict guidelines and protocols for the use of AR to protect patient privacy. Additionally, patients should be fully informed about how their data will be used in AR applications and have the right to opt-out if they have concerns about their privacy.
The Ethical Considerations of Using Augmented Reality in Medicine
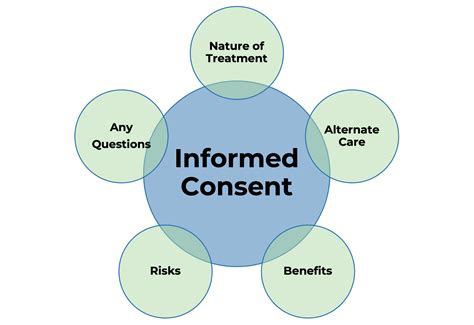
One of the primary ethical considerations when using augmented reality (AR) in a medical setting is the implications for informed consent. AR technology has the potential to provide patients with a more detailed understanding of their medical conditions and the proposed treatments, but it also raises questions about how much information patients can truly comprehend and whether they are able to make fully informed decisions.
Additionally, there is the issue of how AR might alter the traditional process of obtaining informed consent. With the introduction of virtual reality simulations and immersive experiences, patients may be exposed to a level of information that is overwhelming or that could potentially sway their decision-making in ways that are not conducive to truly informed consent.
Furthermore, there is the concern of how the use of AR may impact the autonomy of the patient in the informed consent process. The immersive nature of AR experiences could potentially blur the lines between the patient’s own decision-making and the influence of the technology, raising complex ethical questions about the true extent of patient autonomy in consenting to medical procedures.
| Implications for Informed Consent |
|---|
| Increased level of information |
| Altered consent process |
| Impact on patient autonomy |

The Ethical Considerations of Using Augmented Reality in Medicine
When it comes to the use of augmented reality in the medical field, one of the most important considerations is the potential impact it may have on the doctor-patient relationship. With the integration of AR technology in healthcare, there is a possibility of a shift in the dynamics of this crucial relationship.
Firstly, the introduction of AR devices during medical consultations and procedures may create a barrier between the doctor and the patient. The use of technology in the patient’s presence can make the interaction seem impersonal and less empathetic. This could detrimentally affect the trust and communication between doctors and their patients, leading to a breakdown in the relationship that is essential for effective healthcare delivery.
Furthermore, there is a concern that the reliance on AR technology may cause physicians to prioritize the technology over direct interaction with their patients. This shift in focus could result in a lack of holistic care and a diminished understanding of the patient’s individual needs, preferences, and fears. It is crucial to navigate the use of AR in a way that enhances the doctor-patient relationship rather than hinder it.
Therefore, it is imperative for healthcare professionals and organizations to carefully consider the potential impact of augmented reality on the doctor-patient relationship and take proactive measures to ensure that the human connection and empathy at the core of healthcare are not compromised by technological advancements.

When discussing the use of augmented reality (AR) in the medical field, it’s crucial to consider the implications for equitable access. As with any new technology, there is a risk that it may exacerbate existing health disparities if it is not implemented thoughtfully.
One of the major considerations for equitable access to AR in medicine is ensuring that the technology is affordable and available to all patients, regardless of their socioeconomic status. This means working with healthcare providers and insurers to make sure that AR tools are covered by insurance and are not prohibitively expensive for patients.
Another important aspect of equitable access is ensuring that healthcare facilities in underserved areas have access to AR technology. This may require investment in infrastructure and training for healthcare professionals in these areas to ensure that they can effectively utilize AR tools to benefit their patients.
Finally, it’s important to consider the potential cultural and language barriers that may arise when implementing AR in healthcare settings. Ensuring that AR tools are accessible to patients who speak different languages or come from diverse cultural backgrounds is essential to promoting equitable access.

What are some potential ethical considerations of using augmented reality in medicine?
Some potential ethical considerations include patient privacy, data security, informed consent, and potential biases in the technology.
How can augmented reality impact patient privacy in the medical field?
Augmented reality can potentially compromise patient privacy by displaying sensitive medical information in a way that may be visible to others, posing a risk to confidentiality.
What are the implications of data security when using augmented reality in medicine?
Data security is a significant concern when using augmented reality in medicine as it involves the storage and transmission of sensitive patient information, requiring robust security measures to prevent unauthorized access.
What role does informed consent play in the ethical use of augmented reality in medicine?
Informed consent is essential in using augmented reality in medicine, as patients must be fully aware of how their information is being used and have the opportunity to consent or decline participation in such technology.
How can augmented reality technology introduce potential biases in medical treatment?
The use of augmented reality technology may introduce biases by influencing how medical information is presented to healthcare professionals, potentially impacting decision-making and treatment approaches.
What are some ways to mitigate ethical concerns when using augmented reality in medicine?
Mitigating ethical concerns can involve implementing strict data protection measures, ensuring informed consent from patients, and regularly evaluating and addressing potential biases in the technology.
What are the benefits of using augmented reality in the medical field despite ethical considerations?
Despite ethical considerations, augmented reality in medicine can offer benefits such as improved surgical precision, enhanced medical training, and innovative patient care experiences.